
Greater Horn of Africa
Greater Horn of Africa (Djibouti, Ethiopia, Kenya, Somalia, South Sudan, Sudan and Uganda), Grade 3 Emergency
- Estimated Total Population: 294 million (World Bank)
- Acutely Food Insecure Population (high level): 46.3 million (IPC 3+ crisis or worse)
- Number of Refugees: 4.5 million (UNHCR)
- Internally Displaced People: 13.5 million (UNHCR)
- Estimated acutely malnourished children (under 5 years): 1.8 million (Somalia), 1.4 million (South Sudan), 884k (Kenya) and 104K (Uganda)
- Estimated severely acute malnourished children (under 5 years): 514k (Somalia), 346k (South Sudan), 223k (Kenya) and 16.5k (Uganda).
- WHO steering 4 health clusters and coordinating 262 partners in service of 21.5 million people (Ethiopia, Sudan, South Sudan and Somalia)
- Attacks on health care: 73 attacks, 113 injuries, 93 deaths (Jan 21-Dec 22 in 3 countries)
- Under- five mortality rate (per 1,000 live births, IGME 2020): Somalia 115, South Sudan 98, Sudan 57
- Ongoing outbreaks as of 16 December 2022: Measles (6 countries), Cholera (4 countries), Yellow Fever (2 countries), Mpox, Hepatitis E, Polio, Dengue, Anthrax, Malaria, Ebola disease (caused by Sudan virus)
- Funding requirements: US$ 178 million (Jan-Dec 2023)

Mohammod receives care from midwife Mimi Wasse, a member of the Eltomale Site Mobile Health and Nutrition Team in Chifra, Afar in Ethiopia. Mohammod came to be tested for malaria after having a high fever for a few days.
Context
The Greater Horn of Africa is one of the world’s most vulnerable geographical areas in relation to impacts of climate change and is currently experiencing one of the worst food insecurity situations in decades. It is estimated that more than 46 million people are in Integrated Food Security Phase Classification (IPC) Phase 3 or above.
The sub-region is home to a large pastoralist population with significant vulnerabilities. Currently, the region, which includes Djibouti, Ethiopia, Kenya, Somalia, South Sudan, Sudan and Uganda is experiencing rising food insecurity due to extreme climate events such as drought and flooding, as well as conflict, socio-economic impacts of the COVID-19 pandemic, and volatile food and fuel prices, all of which are contributing to the creation of a huge humanitarian crisis. Regardless of future rainfall performance, the recovery period from a drought this severe will take years, with extremely high humanitarian needs even set to increase in 2023.
As malnutrition increases both the likelihood of falling sick and the severity of disease1, a food crisis is therefore a health crisis. In addition, sick people become more easily sick. Many people must choose between food and health care, with serious implications both for conditions that need long-term treatments, such as tuberculosis (TB) or human immunodeficiency virus (HIV) and non-communicable disease, but also for routine preventive health care services - including for reproductive, maternal and child health – with grave consequences. Disruptions in access to health care can further increase morbidity and mortality, as fragile livelihoods force communities to modify their health-seeking behavior and prioritize access to immediate life-saving assets such as food and water. In addition, displacement often further interrupts utilization of health care services, including preventive services like vaccinations.
More than 46 million people across the region are estimated to be in a ‘crisis’ situation (IPC 3 or worse), within which approximately 275 000 people across Somalia and South Sudan are experiencing a ‘catastrophe’ (IPC phase 5) situation.
In areas affected by food insecurity, outbreaks of communicable diseases are a major public health concern, particularly against a backdrop of often low immunization rates (exacerbated by the COVID-19 pandemic), insufficient health service coverage and the devastating combination of malnutrition and disease. Pregnant and lactating women, newborns, children, the elderly, and people living with chronic diseases such as tuberculosis (TB) and human immunodeficiency virus (HIV), are particularly vulnerable.
While finding food and safe water is a priority, health considerations are essential to avert preventable disease and death. Lastly, the region is largely affected by the continued upsurge of outbreaks of infectious diseases, including cholera, measles, yellow fever, mpox, hepatitis E, dengue, malaria and Sudan Virus disease (SUVD) Ebolavirus disease, which WHO considers to be a major concern. Extreme weather events, massive displacement, food insecurity and malnutrition, limited access to health care and low immunization rates all contribute to an increasing risk of disease outbreaks.
Based on WUENIC (WHO/UNICEF) estimates for the last three years, the routine immunization coverage has been below the expected target, especially in Djibouti, Ethiopia, Somalia, and South Sudan, as a result of conflict, the COVID-19 pandemic, and displacement, fueling the risk of disease outbreaks, which are already a public health concern in areas affected by drought and flooding. Additionally, large-scale displacement may hamper surveillance for epidemic-prone diseases, as well as routine immunizations, further worsening the situation. These health risks clash with an already fragile health system.

Medhne with her child Aron in Um Rakuba Refugee camp in eastern Sudan on 18 August 2022. Medhne lives with six family members and two kids in a small hut. “Even though we live near the clinic, we still have to walk very long distance to the other clinic at the gate of the camp to try to find the prescribed medicine,” she said.
Regional priorities
Health is an essential component of the response to the ongoing emergency, in preventing, reducing, and reversing the causal relationship between poor nutrition, disease and death. As part of ongoing efforts to prevent and respond to food insecurity, WHO will ensure the seamless supply of high-quality critical medicines including contingency stockpiles. Also, WHO and its partners will deliver emergency services to people in need either directly or through local partners, placing emphasis on hard-to-reach areas. In addition, WHO aims to improve national capacities for a more rapid, effective, and resilient health system response.
Emphasis will be placed on vulnerable populations, especially women and children, the elderly, pastoralists, internally displaced persons (IDPs), refugees, persons with disabilities and those with underlying health conditions, such as HIV/AIDS.
Where possible, WHO’s emergency response will build on the existing health infrastructure and its network of partners and community resources. WHO leads the coordination through Health Clusters and other coordination mechanisms among health sector partners and will continue to support health authorities, UN and NGO partners to deliver a package of high-impact interventions to address food insecurity among affected communities, particularly targeting IDPs, refugees, children under five years, newborns, and pregnant and lactating women. WHO will also safeguard the provision of an essential health services package, to encompass maternal and newborn health, immunization, nutrition, mental health and gender-based violence (GBV) services, ensuring implementation of infection prevention and control measures and water quality monitoring at health facilities. A taskforce based in Nairobi will continue to organize and lead its multi-country response and provide technical support to countries in the region.
A key priority for WHO is to ensure high quality health information to guide response efforts to where they are needed most. This includes ensuring the integration of nutrition into health surveillance, alongside strengthening disease surveillance, including early warning and alert systems, and building mortality surveillance. WHO will work with Member States and partners to further advance capacity in this field. WHO will also identify the availability and use of essential health and nutrition services, address barriers to access and analyze the capacity of the health system to cope. This intelligence helps to steer resources for an early response to save life and enable an efficient and informed response.
Further, WHO will put emphasis on outbreak prevention and control, working with its partners on the analysis of surveillance data to support evidence-based interventions. WHO will support the implementation of preventive actions, such as immunization measures as well as field investigations for outbreak verification and response. Importantly, WHO will ensure procurement and pre-positioning of key supplies for outbreak response.
Above-mentioned priorities are complemented by stringent Protection from Sexual Exploitation, Abuse and Harassment (PSEAH) measures: across the region, WHO has a zero-tolerance approach to sexual exploitation and abuse and abides strictly to the Secretary General Bulletin (2003/13) and to the IASC 6 core principles. To ensure this, several measures were implemented in the drought and floods emergency response in 2022 and will be extended and upscaled in 2023.
To date, dedicated PSEAH focal points have been assigned to all 7 countries to ensure key activities are implemented to prevent and to respond to SEA, including training for staff, effective reporting mechanisms and mindful communication with the community. To facilitate and coordinate PSEAH related activities on country level, a PSEAH expert based in the Nairobi hub provides technical support and mentorship to the countries. In 2023, activities will focus on ensuring training for all frontline staff involved in the emergency response, which enables a solid system allowing for prevention and response measures when it comes to sexual exploitation and abuse (SEA). Also, there will be activities rolled out with focus on beneficiaries ensuring their involvement in developing appropriate response and prevention to SEA, and to customize reporting mechanisms which work for beneficiaries in different countries and contexts.
Response pillars



Temira is pictured with her 12-month-old daughter Zahara in front of the Eltomale Site Mobile Health and Nutrition Team in Chifra, Afar in Ethiopia. "This clinic is located near my home, so I can bring Zahara here easily," she said. "Zahara received a check-up and vaccination today. When I am not feeling well, I also come here."
Focus countries
Djibouti
- Estimated total population (World Bank): 1 million
- Acutely Food Insecure Population – high level (IPC3+): 192K
- Number of Refugees (UNCHR): 37K
- Internally Displaced (UNCHR): 6k
- Ongoing outbreaks (WHO): Measles
Djibouti has been facing a persistent drought which has left 400,000 people in need of humanitarian assistance and has had major consequences on health, nutrition, and food security. Up to 50% of Djibouti’s traditionally rural population’s livestock has been lost, and according to the national rapid assessment, 54% of the rural households faced inadequate food consumption.
The drought continues to aggravate pre-existing vulnerabilities and the health consequences on children are severe. Global acute malnutrition (GAM) is prevalent among children under five years of age living in rural settings. The admission trends of children admitted to health posts and clinics and receiving treatment for Severe Acute Malnutrition (SAM) has increased by approximately 26%.
WHO and its partners continue to implement surveillance and response programs, which aim to prevent and cure most non-communicable and communicable diseases including malaria, measles, and polio.
Key results in 2022:
- More than 39,000 children vaccinated against measles (90% coverage) and more than 158,000 under-fives reached through a polio vaccination campaign.
- Eight surveillance focal points deployed to strengthen nutritional surveillance and response activities.
- Expert nutritionists were deployed to strengthen nutritional surveillance and response activities and to improve general quality of medical care for management of SAM.
- Supported MoH in strengthening surveillance activity by providing training to health personnel on sample collection and shipment.
- Established a surge team to support the emergency response; deployed 7 nutrition focal points in six regions.
- Focus on quality assurance of vaccination campaigns and improved health information management through provision of technical experts.
- Nutritional kits (13 SAM/MAM kits), and essentials (therapeutic milk, F75, and F100) were distributed.
Ethiopia
- Estimated Total population (World Bank): 118 million
- Acutely Food Insecure Population- high level (IPC3+) (OCHA HRP 2022): 20.4 million
- Number of Refugees (UNCHR): 876k
- Internally Displaced (UNCHR): 4.6 million
- Ongoing outbreaks (WHO): Measles, Cholera, Malaria, Polio, Anthrax, Dengue and Chikungunya
Ethiopia is currently experiencing one of the worst drought crises, resulting from delayed and sub-optimal rains for the last five seasons. This has affected at least 17 million people living in the drought affected areas of Somali, Oromia, Afar, Southern Nations Nationalities and People's Region (SNNP) and regions found in the eastern and southeastern parts of the country. Severe water shortages and loss of livestock have led to several thousand people migrating in search for resources including water, food, health and nutrition services. This situation is associated with a significant deterioration in food security, the disruption of essential health services, including routine immunization services, increasing levels of acute malnutrition, and disease outbreaks such as measles, malaria, cholera, meningitis and diarrheal diseases. There is limited capacity and preparedness activity implemented in the drought-affected areas to respond to outbreaks.
Among the reported effects are increased risk of infectious diseases, such as cholera, diarrhea, and pneumonia, lack of water and sanitation, displacement, psycho-social stress and mental health disorders, and disruption of local health services due to a lack of water supplies. WHO and its partners have been able to provide some humanitarian support to affected communities, but is affected by resource and access constraints, resulting in about 51% of the drought-affected areas being without health partners.
Key results in 2022:
- 233.7 metric tons of emergency health kits (IEHK, pediatric SAM, cholera kits) distributed to the Ministry of Health (MoH) to increase health care management capacity in drought-affected areas.
- Supported implementation of reactive measles vaccination campaigns.
- Trained 736 health workers on severe acute malnutrition management, 120 health workers on gender-based violence and 305 health workers on MHPSS.
- Over 470 Rapid Response teams trained to strengthen surveillance and outbreak response.
- Surveillance officers deployed to support the MoH to strengthen case identification, reporting and outbreak response.
- Supportive supervisions conducted at 40 health facilities to improve and streamline the disease surveillance and reporting activities.
Kenya
- Estimated Total population (World Bank): 55 million
- Acutely Food Insecure Population- high level (IPC 3+): 4.4 million
- Acutely Malnourished Children (Estimated, IPC): 884k
- Ongoing outbreaks (WHO): Measles, Cholera, Chikungunya, Yellow fever
Kenya is facing a protracted drought that has been ongoing since 2021. It is projected that 4.35 million people will be in need of humanitarian assistance in 2023. The worsening food security situation in 2022 has resulted in acute malnutrition rates across the country, with 942,000 children aged 6-59 months acutely malnourished and 134,000 cases of pregnant or lactating women acutely malnourished and in need of treatment. The situation has resulted in communities becoming more vulnerable, with deaths in some counties, and surges in disease epidemics including most recently cholera, chikungunya, dengue fever, along with deaths related to yellow fever and visceral leishmaniasis.
Access to adequate essential health services continues to impact regions with remote health facilities leading to under-utilization of static health facilities and reduced health service delivery approaches, such as integrated outreaches. The worsening severe acute malnutrition (SAM) rates are impacting the health status of children and women, with deaths reported in some counties, and an increase in disease outbreaks. Women of reproductive age are increasingly experiencing pregnancy-related complications and limited access to family planning information and services.
Key results in 2022:
- In collaboration with the MoH, WHO chaired the development of the national drought response operational plan and the strategic response plan for 2023 for a coordinated and response.
- In partnership with the MoH, WHO improved the early warning system in disease detection and monitoring and strengthening community-based surveillance network (CBS) in counties with high risk of Ebola outbreak.
- IMAM (Integrated Management of Acute Malnutrition) training supported in 9 counties - 687 HCWs have been trained.
- Procurement of RUTF - 5 000 BOXES of 150 sachets (92 g) - to be shipped to Kenya in December.
- Screening of children for malnutrition and referral for treatment in OTP and SC sites.
- Distribution of IEHK kits – 1 334 Basic Module and 548 Basic equipment, (35 cholera Kits, 500 additional IEHK).
- Mapping of health facilities and outreach sites ongoing in the counties to increase access to health services.
- WHO is leading on the ongoing response to the different outbreaks like measles, cholera and yellow fever through capacity building on surveillance and case management as well as in provision of essential drugs and supplies for outbreak control.
Somalia
- Estimated total population (World Bank): 16.9 million
- Acutely Food Insecure Population- high level (IPC 3+): 6.7 million
- Number of Refugees (UNCHR): 51.4K
- Internally Displaced (UNHCR): 3.1 million protracted IDPs and 752,000 newly displaced
- Acutely Malnourished Children (Estimated, IPC) 1.8 million
- Ongoing outbreaks (WHO): Measles, Cholera
Somalia is experiencing one of the worst droughts in its history due to poor rainy seasons and related water shortages. Decades of conflict, frequent epidemics of cholera and measles, widespread poverty, and recurrent climatic shocks, including the ongoing drought emergency, continue to weaken and cause widespread fragility to the health systems in Somalia. Approximately 8.3 million people across Somalia are expected to face Crisis (IPC Phase 3) or worse acute food insecurity outcomes between April and June 2023. Famine (IPC Phase 5) is projected between April and June 2023 among agropastoral populations in Baidoa and Burhakaba districts of Bay region and among internally displaced people (IDP) in Baidoa town of Bay region and in Mogadishu. These areas are already experiencing very high levels of acute malnutrition and mortality consistent with Emergency (IPC Phase 4) outcomes. In addition, an increasing number of people are expected to be in Catastrophe (IPC Phase 5) in multiple other areas across Somalia through mid-2023. The total estimated acute malnutrition burden in Somalia is expected to reach approximately 1.8 million children, including 513,550 children who are likely to be severely malnourished, through July 2023.
Women and children continue to endure adverse health and nutrition effects the most. With an estimated 6.7 million people already in need of urgent humanitarian assistance and protection, and an estimated 3.1 million internally displaced persons, Somalia has the highest number of internally displaced people in the world.
Increased incidences of waterborne diseases, especially cholera and acute diarrhea, are seen among drought-affected populations. Currently the country is experiencing multiple disease outbreaks including measles, cholera, and dengue fever, resulting in an increase in morbidities and mortalities.
Key results in 2022:
- Improved early warning system for disease detection and monitoring and strengthen the CBS network focused on the priority districts (IPC level 3-4-5).
- Ongoing support to rapid response team (RRT) at national and sub-national level, supporting outbreak/alert investigation and the early warning system in disease detection and monitoring.
- Increased distribution of SAM kits to 64 stabilization centers supported in priority areas and enhanced capacity of outreach teams to detect, care for and refer malnourished children in hard-to-reach areas.
- Ongoing coordination on inter-agency Integrated Response Framework response in hard-to-reach areas.
- Ongoing collaboration with 53 health cluster Partners – 17 of 19 regions, 61 of 74 districts. Between March and November 2022, WHO and Health Cluster Partners have reached out to 71% of the population (over 6.5 million people) affected by the severe drought with life-saving healthcare support, including vaccination.
- Acceleration of the ongoing cholera outbreaks response: OCVs campaigns were conducted (950k people received) and 1 million more doses arrived in December 2022 for further campaigns, increased supply of cholera kits for cholera treatment centres and additional training and support is rolled out by WHO in hotspots: Outreach teams deployed with capacity to detect, care and refer including first line responders.
- Supporting ongoing measles outbreak response - Targeted campaigns done and nationwide integrated campaign finalized in December with 2.3 M children between 6 months to 5 years old vaccinated against measles and 2.6 M children (0-59 months) against polio. This campaign involved distribution of Vitamin A (2 million children) and deworming (1.8 million children).
- Outreach services set up in 54 districts to strengthen routine immunization, screen for malnutrition with referral capacity, and distribute micronutrient supplements with focus on children.
Also, the country, by December 2022, has achieved 40% of its people fully vaccinated against COVID-19, a sign of building resilience for immunization system in the country.
Somalia is not only facing a prolonged drought and humanitarian emergency, but the country is also facing security challenges. WHO Somalia is responding to these events too. WHO and its partners extended life-saving support to twin-blast victims of Mogadishu.
South Sudan
- Estimated Total population (World Bank): 11.4 million
- Acutely Food Insecure Population-high level (IPC3+): 6.3 million
- Number of Refugees (UNHCR): 341k
- Internally Displaced (UNHCR): 2.2 million
- Acutely Malnourished Children (Estimated, IPC) 1.4 million
- Ongoing outbreaks (WHO): Cholera, Measles, Hep E, Malaria and Anthrax
South Sudan continues to face multiple concurrent crises, including high levels of food insecurity, inter-communal violence, conflict, extensive flooding, and disease outbreaks that have persisted for years. In 2023, the food insecurity situation is likely to deteriorate, with 6.3 million people (51% of the population) projected to become highly food insecure, worsened by a fourth year of continued flooding.
South Sudan continues to be in a state of nutrition emergency with a global acute malnutrition (GAM) rate in some states above the WHO classification of 15 %, as indicated in the last Food Security and Nutrition Monitoring System (FSNMS). A critical nutrition situation exists in all the three conflict states of Upper Nile, Jonglei and Unity and other states in Greater Bahr El Gazal (Warrap and Northern Bahr El Gazal) and Equatoria (EES) region. Access to health services is a major challenge, particularly amongst displaced populations. Even in settlements with access to a health facility, functionality and quality of care remain a challenge. Utilization of health services continues to fall below the minimum threshold amongst the general population.
Key results in 2022:
- Reactive vaccination campaigns conducted in 16 counties, targeting children aged 6 months to 14 years – a total of 77 0581 children received measles vaccines.
- Two rounds of OCV campaigns (against cholera) were conducted – more than 1.6 million doses were administered in six cholera hotspot and flood-affected areas.
- Distributed 2 151 Interagency Emergency Health Kits (IEHK), and 100 severe acute malnutrition (SAM) with medical complication kits.
- 198 health care workers were trained (99 on nutritional surveillance, reporting in EWARS and 99 on in-patient management).
- 828 frontline health workers were trained (312 on case management, 210 community-based case management/BHWs, 230 on IDSR, 39 on RRTs, 37 on laboratory sample management).
Sudan
- Estimated Total population (World Bank): 45 million
- Acutely Food Insecure Population-high level (IPC 3+): 11.7 million
- Number of Refugees (UNHCR): 1.1 million
- Internally Displaced (UNHCR): 3.7 million
- Ongoing outbreaks (WHO): Measles, Mpox, Malaria, Hepatitis E, Polio and Dengue Fever
Sudan has been affected by the combined impact of prolonged dry spells and crop failure across 14 states, which has impacted over 5.6 million people. Overall, 3.1 million people need short to long-term assistance and more than 22 million people (50% of Sudan’s population) live in the 115 dry spell-affected localities. An increase in localized conflicts has triggered population displacement, which, combined with the deterioration of the economy, has led to higher than usual levels of acute food insecurity. As a result, the highest prevalence of population in Crisis (IPC Phase 3) or worse are observed in North Darfur (25%), followed by West Darfur (22%), North Kordofan (20%), South Kordofan (20%), Gedarif (19%) and Central, East and South Darfur states, ranging from 17-18%.
Sudan also hosts over 1.14 million refugees, including 763 000 South Sudanese refugees and 61,000 Ethiopian refugees, and is a key transit country for migrant populations that are already at increased risk of epidemic-prone disease.
By the end of 2022 Sudan reported multiple severe disease outbreaks such as mpox, dengue fever, malaria, measles on top of the ongoing COVID-19 pandemic.
At the beginning of 2022, the Sudan Humanitarian Needs Overview (HNO) estimated that over 3 million children under-five were acutely malnourished and in need of lifesaving humanitarian nutrition assistance. Humanitarian partners estimate that with various challenges and factors that underpin conflict and displacement not resolved, the number of people who need assistance is likely to increase further in 2023.
Key results in 2022:
- WHO spearheaded and interagency rapid needs assessment and missions to flood-affected states
- Deployed STC epidemiologist and data management officer and strengthened epidemiological surveillance (IBS, CBS) and built RRTs capacities for EVD and MPX - trained >500 surveillance staff, >800 CHWs, and 210 RRTs members
- Supported the Pandemic Influenza Preparedness Training and endorsement of PIP National documents and updated the national Laboratory policy 2022
- Ongoing support to 51 vector sentinel surveillance sites, source reduction, and health promotion activities in 9 States
- Supported MoH to strengthen indicator-based and community-based surveillance
- Ebolavirus disease (EVD) preparedness and risk assessment exercises conducted across all 18 states and finalized the national EVD preparedness plan followed by:
ONE HEALTH mpox outbreak response missions in four states with participation of human, animal and environmental sector experts.Intra state deployments of experts with technical support from WHO Sudan for dengue fever outbreak response continued water quality monitoring and surveillance in 13 states supporting 51 vector sentinel surveillance sites on source reduction, health promotion activities in nine states.
Supported the integrated vector control outbreak response measures - 40 technical MoH staff and 147 community volunteers trained on IVM and On job training for 170 community volunteers on Aedes mosquito control.
Procurement of drugs, laboratory supplies (RDTs, Reagents), and PPEs - IEHKs (5), TESKs (101), SAM kits (12), Cholera Kits (6)
Uganda
- Estimated Total population (World Bank): 47.1 million
- Acutely Food Insecure Population – high level (IPC 3+): 315k
- Number of Refugees (UNHCR): 1.5 million
- Acutely Malnourished Children (Estimated, IPC): 104k
- Ongoing outbreaks (WHO): Sudan virus disease, Measles, Polio, Yellow fever, Anthrax and Malaria
Uganda’s population mainly resides in rural areas, with their livelihoods based on livestock (nomadic pastoralism) and crop production. Karamoja region, located in the northeast of Uganda, is one of the poorest regions in Uganda and continues to have the highest food insecurity and malnutrition levels in the country, due to inadequate food access, extreme weather/prolonged drought, pest infestation, poor feeding practices, structural poverty, poor hygiene and sanitation, and morbidity. malaria and diarrhoea cases are still high in the region, which places a high disease burden on children, leading to malnutrition.
The national economy faces high food prices, commodity shortages and restrictive measures to combat inflation, all of which complicate the outlook in Karamoja region and the adjoining districts. Across Karamoja and the surrounding districts, the quality of care for children with severe acute malnutrition (SAM) remains below WHO recommended standards. Despite current support from WHO, the coverage and quality of care from SAM treatment remains a key priority.
Key results in 2022:
- 499 health workers were trained in surveillance and outbreak response (IMAM, Tuberculosis, Basis Emergency Obstetric Care (BEmOC), and PSEAH)
- A reactive vaccination campaign against measles conducted in the Lamao district, reaching 17 626 children aged from 6 months to 14 years.
- Deployment of 12-bed capacity mobile units for the acute management of SAM cases in Moroto.
- Supported the scale-up of active case detection of TB, Karamoja region has the highest cases of TB among children under 5 years which also adversely affects effective treatment of acute malnutrition
- Procurement of essential medical supplies
- WHO in collaboration with the Hungarian Government deployed a 12-bed capacity mobile unit for case management of SAM cases in Moroto
- Supported establishment of 3 field hubs (Moroto, Soroti and Gulu); and trained a total of 46 staff (Recruited 20, repurposed 26) to enable aid in remote areas.
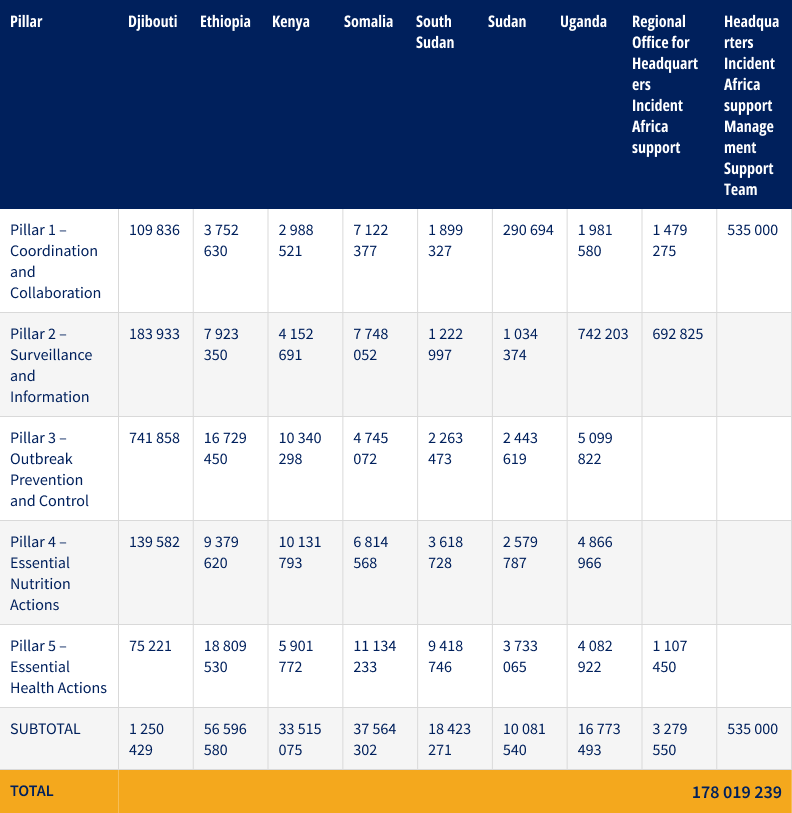
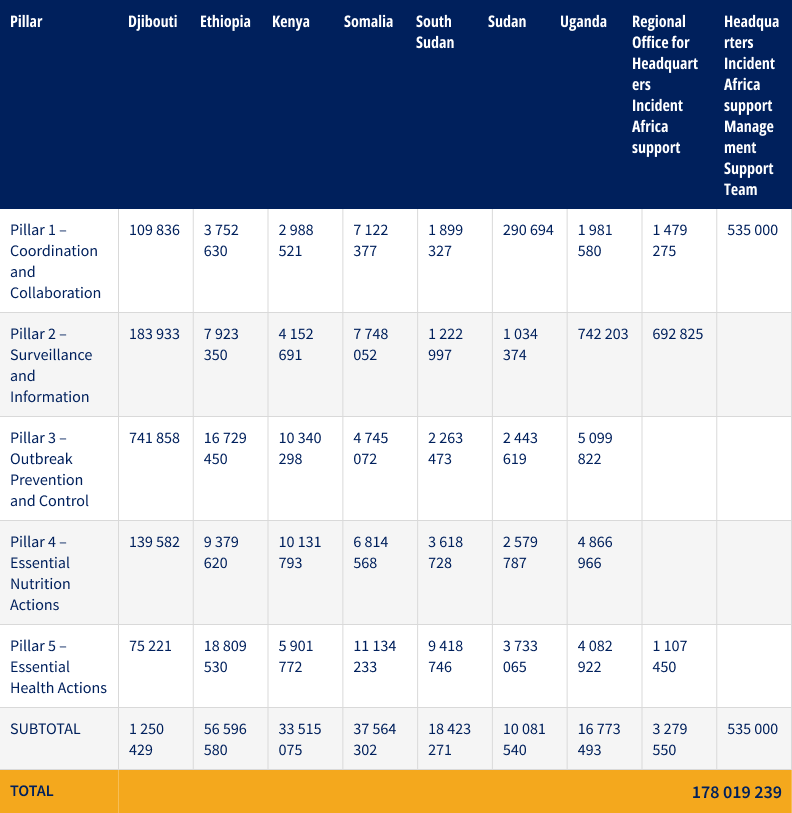
Funding requirements
Overall country funding requirements, including COVID-19, by pillar (US$)
For more information

